- The new NCEP III provides revised guidelines for the treatment of hyperlipidemia.
- Combining traditional risk factor assessment with the calculated 10-year risk of coronary artery disease allows for optimal patient-centered counseling.
- Statins are normally the first-line therapy for hyperlipidemia.
In 1995 and 1996, US adults made more than 18 million office visits for the evaluation and treatment of hyperlipidemia, including 3.4% of all visits to family physicians. Among visits to family physicians, 4.1% included measurement of cholesterol levels.1 Overall, mean cholesterol levels decreased from 220 in 1960–1962 to 203 in 1988–1994. During the same time period, the proportion of adults with elevated total cholesterol levels (> 240) decreased from 32% to 19%.2 Despite this progress, the availability of more effective drugs, guidelines advocating increasingly aggressive treatment, and populationwide goals established in Healthy People 2010 will continue to increase the number of patients seen by family physicians for screening, diagnosis, and treatment of hyperlipidemia.3
When to treat
The National Cholesterol Education Program (NCEP), a program within the National Institute of Health’s Heart, Lung, and Blood Institute, published a guideline in 1993 for screening and treating hyperlipidemia. Physicians have since become familiar with the NCEP concept of basing treatment decisions on assessment of patient risk factors (smoking, age, diabetes, hypertension, family history of early coronary artery disease [CAD]) and application of algorithms linked to desired low-density lipoprotein (LDL) cholesterol levels. The advantage of this strategy is its simplicity. Physicians assess whether the NCEP risk factors are present and then work with their patients to achieve the desired LDL level through lifestyle modification, drug therapy, or both.
Unfortunately, the NCEP guideline did not assess the individual’s actual risk of CAD. In its recently released Third Report, the NCEP has recognized the value of this strategy by incorporating the Framingham tables to calculate the 10-year risk of developing clinical CAD based on a patient’s individual risk factors, including cholesterol levels (Table 1).4 This new NCEP III guideline recommends traditional risk factor counting coupled, in certain situations, with the 10-year risk derived from the Framingham scoring system.
TABLE 1
FRAMINGHAM TABLES FOR CALCULATING CORONARY ARTERY DISEASE RISK
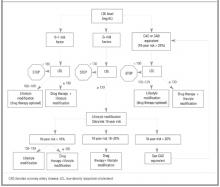
Therapy is based on the individual patient’s risk category and LDL levels (Figure). Patients whose 10-year risk is greater than 20% or those who have CAD-equivalent conditions (ie, diabetes, peripheral arterial disease, abdominal aortic aneurysm, symptomatic carotid artery disease) are considered to have a risk equivalent to that of patients with known CAD; all have an LDL goal of 100 or less.
For those with a 10-year CAD risk less than 20%, the number of positive risk factors determines the LDL goal. This new method allows physicians to communicate with their patients more clearly about individual risk and enhances shared decision making. While the NCEP III report is based on extensive literature review, the recommendations of its expert panel are not characterized according to the strength of the supporting evidence, as is done by the US Preventive Services Task Force.
Figure
TREATMENT STRATEGY BASED ON LDL LEVEL AND RISK CATEGORY
Explaining treatment benefits
The NCEP III report does not make explicit the effect of the treatment on the patient; that is, how much the proposed treatment will reduce the risk of CAD. This determination depends in part on whether the patient being treated has known CAD or a CAD-equivalent condition (secondary prevention) versus no known CAD (primary prevention). The benefits of treatment have been most clearly quantified for drug treatment and are most easily evaluated using the number needed to treat (NNT). The NNT refers to the number of patients who would have to be treated for 5 years to prevent 1 CAD event. Physicians may use the NNTs to assist patients in determining their preferences for treatment, bearing in mind that the NNT refers to an outcome for a population, such as men with high cholesterol levels. For a given individual, their risk of an adverse outcome is all or none. Nonetheless, patients may find the NNT a useful way to assess their personal values in making treatment decisions.
Treatment
Lifestyle modification
Diet modification is the cornerstone of therapy for mild to moderate hyperlipidemia. Modifying the diet is also recommended along with pharmacologic therapy in people at higher risk of CAD. NCEP III recommends a diet for “therapeutic lifestyle changes” that includes < 200 mg cholesterol per day, < 7% saturated fat, 25% to 35% total fat, 50% to 60% carbohydrates, and 15% protein of total calories.4