Can you name these 2 nail conditions?
What underlying diseases do you suspect are behind these conditions?
If you said onycholysis (left) and red lunula (right), you are correct. As for the underlying diseases: The patient with onycholysis has hyperthyroidism and the patient with red lunula has chronic obstructive pulmonary disease (COPD). Onycholysis and red lunula are among the more common changes to the morphology (shape) and color of the nail—the 2 ways by which nail changes are classified.
Nail abnormalities can be a revealing sign of underlying disease, and because the nails are readily examined, a convenient diagnostic tool, as well.
This review of common—and not so common—nail disorders shows which changes to the nail are more likely to occur with which underlying internal diseases.
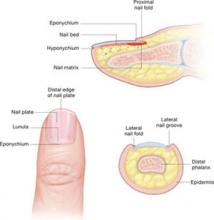
Nail anatomy
Nail changes are classified according to whether they occur in the morphology (shape) or color of the nail. Onycholysis, clubbing, and koilonychia are some of the most common changes in the morphology of the nail. Red lunula is one of the most common changes in the color of the nail.
- Amyloid and multiple myeloma
- Anemia
- Bronchiectasis
- Carcinoma (lung)
- Erythropoietic porphyria
- Histiocytosis X
- Ischemia (peripheral)
- Leprosy
- Lupus erythematosus
- Neuritis
- Pellagra
- Pemphigus vulgaris
- Pleural effusion
- Porphyria cutanea tarda
- Psoriatic arthritis
- Reiter’s syndrome
- Scleroderma
- Syphilis (secondary and tertiary)
- Thyroid disease
What you’ll see: Distal separation of the nail plate from the underlying nail bed. Nails with onycholysis are usually smooth, firm, and without nail bed inflammation. It is not a disease of the nail matrix, though nail discoloration may appear underneath the nail as a result of secondary infection.
What to suspect: Onycholysis is associated with many systemic conditions, including thyroid disease—especially hyperthyroidism. (See list at left.) The nail changes seen with hyperthyroidism usually consist of onycholysis beginning in the fourth or fifth nail, the so-called Plummer’s nails.1 Nakatsui and Lin2 have suggested that patients with unexplained onycholysis be screened for asymptomatic thyroid disease.
What you’ll see: Increased transverse and longitudinal nail curvature with fibrovascular hyperplasia of the soft tissue proximal to the cuticle. With clubbing, the Lovibond’s angle, formed between the dorsal surface of the distal phalanx and the nail plate, is greater than 180 degrees. Schamroth’s sign—the disappearance of the normal window between the back surfaces of opposite terminal phalanges—may also be present.3
What to suspect: Clubbing may be hereditary, idiopathic, or acquired in association with a variety of disorders. It may also be unilateral or bilateral. Unilateral clubbing has been associated with hemiplegia and vascular lesions, while bilateral clubbing has been linked to neoplastic, pulmonary, cardiac, gastrointestinal, infectious, endocrine, vascular, and multisystem diseases.
Cribier et al4 studied the frequency of nail disorders in HIV-infected patients and found that clubbing affects 5.8% of these patients. Moreover, Cribier’s data reinforced the notion that clubbing could be an early sign of AIDS in pediatric patients, and thus play a role in diagnosis.
What you’ll see: Concave thin nails with everted edges shaped like a spoon and capable of retaining a drop of water. It is more common in fingernails, but is occasionally seen in toenails.
What to suspect: This nail sign may result from trauma, constant exposure of hands to petroleum-based solvents, or nail-patella syndrome. Koilonychia is most commonly associated with iron deficiency anemia and occasionally occurs in patients with hemochromatosis. Other frequent systemic causes of koilonychia include coronary disease and hypothyroidism.5 In addition, koilonychia is sometimes a normal variant in infants; it usually disappears in the first few years of life.
What you’ll see: Proximal separation of the nail plate from the nail bed. This typically results in shedding of the nail.
What to suspect: Trauma is the usual cause. Less common causes include poor nutritional status, febrile illness, or drug sensitivity.
Wester et al6 observed the development of onychomadesis in a critically ill patient with a large pulmonary abscess. Onychomadesis is often a clinical manifestation of pemphigus vulgaris.7 It has also been associated with Kawasaki disease8 and hand, foot, and mouth disease.9
What you’ll see: Transverse depressions in the nail plate that occur as a result of a temporary cessation in nail growth.
What to suspect: The causes are similar to those of onychomadesis and include trauma, poor nutritional status, febrile illness, and drug sensitivity.
What you’ll see: Pinpoint (or larger) depressions in an otherwise normal nail.
What to suspect: Pitting is usually associated with psoriasis and affects 10% to 15% of patients with the disorder.10 Pitting has also been reported in patients with Reiter’s syndrome (and other connective tissue disorders), sarcoidosis, pemphigus, alopecia areata, and incontinentia pigmenti.5