Patients with sinus headaches have thick nasal discharge, fever, chills, sweats, or abnormally malodorous breath (SOR: B, cross-sectional study).
The 5 symptoms that are most predictive of migraine are: pulsatile quality, duration of 4 to 72 hours, unilateral location, nausea or vomiting, and disabling intensity (SOR: B, retrospective cohort). As the number of these symptoms increases, so too, does the likelihood that the patient has a migraine (SOR: B, systematic review of retrospective cohort studies).
Most patients diagnosed with sinus headache actually have a migraine headache (SOR: B, 2 cross-sectional studies).
EVIDENCE SUMMARY
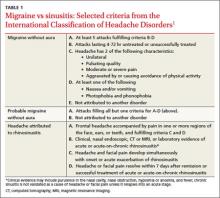
Clinical signs and symptoms define headache types. The International Headache Society (IHS)’s definition of migraine (which is considered the gold standard) includes many of the same symptoms associated with headaches attributed to rhinosinusitis (TABLE 1).1 In order for a headache to be attributed to rhinosinusitis, the patient must meet the definition of acute rhinosinusitis as defined by the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS). The definition includes purulent discharge, nasal obstruction, and facial pain-pressure-fullness.
Migraine headache symptoms include nasal discharge but not purulent discharge or nasal obstruction. The IHS doesn’t accept chronic sinusitis as a cause of headaches unless the patient meets the criteria for acute rhinosinusitis.1,2
When a “sinus” headache isn’t
A cross-sectional study enrolled 100 patients (78 female, 22 male) 18 to 81 years of age who responded to an advertisement seeking people with self-diagnosed “sinus” headaches.3 A neurologist used the 2004 IHS criteria to classify the correct headache type. In 86% of patients, the investigators reclassified the patients with a migraine or probable migraine. Only 3 patients retained the sinus headache diagnosis. All 3 had at least one of the following: thick nasal discharge, fever, chills, sweats, or abnormally malodorous breath. The remaining 11 patients suffered from other headache subtypes.
The big 5 migraine symptoms
A prospective cohort study of 166 French railway employees evaluated the sensitivity and specificity of individual components of the IHS criteria. Patients enrolled had an average age of 39 years and a female-to-male ratio of 1:2. A neurologist diagnosed the headache type and placed patients into either a migraine or nonmigraine cohort. Researchers asked participants about IHS defined migraine symptoms and then compared the frequency of positive responses from migraineurs vs nonmigraineurs.
Five specific IHS criteria were found to be useful in identifying patients with migraine: duration between 4 and 72 hours (odds ratio [OR]=2.5; P=.02), unilateral location (OR=2.3; P=.03), pulsating quality (OR=2.4; P=.02), disturbance of daily activity (OR=2.5; P=.02), and nausea or vomiting (OR=2.8; P=.009). Any 4 of these features indicated a probability of migraine headache of ≥70%. The presence of photophobia and phonophobia (OR=0.5; P=.11) and aggravation by physical activity (OR=1.7; P=.14) didn’t improve diagnostic accuracy.4
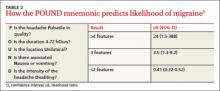
A systematic review of retrospective cohort studies later analyzed the data.5 The authors derived the POUND mnemonic (TABLE 2)5 to aid clinicians in using the 5 clinical features to determine the likelihood of migraine headache. When any 4 of the 5 screening questions are positively, the likelihood ratio (LR) for migraine is 24 (95% confidence interval [CI], 1.5-388). Conversely, when 2 or fewer screening questions elicit positive responses, migraine is less likely (LR=0.41; 95% CI, 0.32-0.52).5
Most “sinus” headaches found to be migraine
A multicenter cross-sectional study evaluated 2991 male and female primary care patients, 18 to 65 years of age, who reported at least 6 self-described or physician-diagnosed sinus headaches within the preceding 6 months.6 At baseline, patients reported the following symptoms: pulsing or throbbing pain (89%), pain that worsened with physical activity (85%), sinus pressure (84%), sinus pain (82%), nasal congestion (63%), photophobia (79%), nausea (73%), and phonophobia (67%). Patients were excluded if they had a previous diagnosis of migraine, used a triptan, had a radiologic diagnosis of sinusitis, or had purulent drainage or fever.
Using the patients’ headache histories, reported symptoms, and the IHS criteria, researchers reclassified 88% of these “sinus headache” patients as having migraine type headaches.
Recommendations
IHS recommends using strict criteria for diagnosing migraines and headaches attributed to rhinosinusitis.1