• Screen for hypertrophic cardiomyopathy (HCM) during preparticipation sports physicals. C
• Patients who have symptoms of, or are diagnosed with, HCM should be cleared by a cardiologist before being allowed to participate in organized sports or engaging in physical exercise. B
• Patients with HCM and a history of cardiac arrest should be given the opportunity to receive an automatic implantable cardioverter defibrillator (AICD). A
• Beta-blockers are first-line therapy for patients with HCM who have symptoms of heart failure. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Hypertrophic cardiomyopathy (HCM) is the most common cardiac genetic disorder.1 But it is best known for its tragic outcomes—the sudden cardiac death (SCD) of young athletes, many of whom are in high school or college.
In fact, HCM can present at any time from infancy through old age, and has a broad range of manifestations. Some individuals remain asymptomatic throughout their lives and enjoy a normal life span; others experience a range of symptoms, from chest pain and dyspnea on exertion to dizziness, light-headedness, palpitations, and syncope. Diagnosis is difficult, and predicting which patients will develop severe complications and face the greatest risk of premature SCD remains an inexact science.
What is clear is that in the United States, HCM causes SCD far more than any other condition.2 HCM has been positively identified in well over a third of cases (36%) of SCD in athletes under the age of 30, and cited as a possible cause in another 8%. Coronary artery anomalies is a distant second, responsible for 17% of sudden deaths in this patient population; myocarditis follows, at just 6%.2
We also know that HCM itself occurs much more frequently than previously believed. In the early 1980s, its prevalence was estimated at <1 in 100,000;3 today, HCM is believed to affect approximately 1 in 500 adults.2,4 Because this potentially fatal condition often remains undetected until an athlete collapses on the playing field, it is crucial that family physicians—who conduct many of the sports physicals typically required before students are permitted to play competitive sports—maintain a high degree of suspicion.
Knowing what signs and symptoms to look for and, perhaps more importantly, the key questions to ask, will help you identify young athletes at risk. This update, which begins with a review of the genetic basis and pathophysiology of HCM, will prepare you to take steps to protect your young patients.
Genetics and pathophysiology
HCM is associated with an autosomal-dominant family of disorders affecting any of 11 genes encoding for proteins in the myocardial sarcomere.5 Hundreds of mutations have been identified that can cause HCM disease. (You’ll find an updated list at http://genetics.med.harvard.edu/~seidman/cg3/index.html.)
The disease occurs equally in men and women,6 although far more males than females die on the playing field.3 Postulated reasons for the lower death rate in female athletes include differences in training regimen; lack of participation in high-risk sports such as football; and, until recently, fewer opportunities for young women to participate in high school and college athletic programs.3 HCM has no known racial predilection, although it may be underdiagnosed in women, minorities, and underserved populations.6
Myocardial tissue is disordered
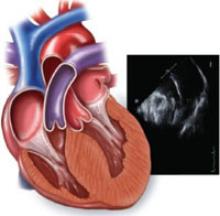
The pathophysiology of HCM directly relates to the disordered myocardial tissue arising from the various gene mutations. Left ventricular myocytes appear hypertrophied and are chaotically arranged in bizarre structural patterns.1,7 This results in asymmetrically thickened and stiff ventricular walls, which can lead to diastolic dysfunction from poor left ventricle filling.
The abnormally thickened walls and septum also push the mitral valve anteriorly during systole. In some HCM patients, the anterior motion of the mitral valve, in conjunction with septal hypertrophy, result in obstruction of the subaortic left ventricular outflow tract. This obstruction—known as left ventricular outflow tract obstruction, or LVOTO—changes with physical position as well as physiological factors such as hydration level, heart rate, and vascular preload, making the murmur and abnormal pulses associated with it hard to detect during a physical exam.6
Ischemia and scarring result
The coronary arteries of patients with HCM are often tortuous, with thickened walls and narrow lumens. This leads to uneven perfusion and areas of relative myocardial ischemia, which result in patchy scarring. The ischemia, disorganized cellular architecture, and myocardial scarring create an environment that promotes the ventricular and atrial arrhythmias that commonly complicate HCM.1