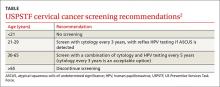
› Screen for cervical cancer in women ages 21 to 29 using cytology alone every 3 years. For women ages 30 to 65, screening with a combination of cytology and human papillomavirus (HPV) testing every 5 years is the preferred option. A
› Be aware of the alternative guideline proposed by several specialty organizations: All women ages 25 to 64 should receive primary HPV screening every 3 years with the FDA-approved HPV test. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
If the cervical cytology report you receive for a woman in her mid-20s is negative, how soon would you plan to repeat testing? Recommendations from the United States Preventive Services Task Force (USPSTF) and other leading organizations advise a combination of cytology and human papillomavirus (HPV) testing at specified intervals depending on a patient’s age. However, a study published in 2015 analyzed data from a statewide registry on provider behavior and found a wide array of screening intervals in practice and infrequent use of HPV testing. 1 Clearly, adherence to published guidelines has been inconsistent.
Now, recommendations by several specialty groups are evolving based on newer evidence regarding HPV testing. These alternative guidelines recommend primary high-risk HPV testing for all women. This change is the topic of much national debate and is being researched for the USPSTF’s 2018 update on cervical cancer screening.
In this article, I review the USPSTF’s present recommendations and look ahead to how “best practices” for cervical cancer screening may be changing.
Current cervical cancer screening guidelines
Many subspecialty organizations and government agencies publish cervical cancer screening guidelines. The USPSTF guidelines, reviewed here, are evidence based, frequently updated, and widely used by primary care providers ( TABLE).2,3 These guidelines recommend initiating cytology testing at age 21 and, if results are normal, repeating every 3 years. Reflex HPV testing is recommended if cytology results reveal atypical squamous cells of undetermined significance (ASCUS). For women ages 30 to 65, the preferred option is to undergo a combination of cytology and HPV testing every 5 years. 2 Women older than 65 may discontinue screening. 2 HPV immunization status does not affect USPSTF recommendations. Nationwide rates of HPV vaccination among females ages 13 to 17 vary among states, from ≤49% to ≥70%. 4
What the guidelines do, and do not, cover. The USPSTF screening intervals apply as long as testing results are normal. 2 These guidelines apply to all women regardless of the age at which they began sexual activity. These guidelines do not apply to women who have had abnormal cytology or HPV results and have not undergone adequate follow-up to ensure their lesion has cleared. 5 These guidelines also do not apply to women who are immunosuppressed, who were exposed to diethylstilbestrol (DES) in utero, who have had a hysterectomy for non-oncologic reasons, or who have had cervical cancer. 5 A woman may stop routine screening after age 65 if she has had adequate follow-up including either 3 negative cytology samples or 2 negative co-tests (cytology and HPV test) in the last 10 years. 6 A woman may also discontinue screening if she has had a total hysterectomy and has no history of cervical dysplasia. 7
Evidence behind the guidelines. The USPSTF guidelines were updated to their current state in 2012 reflecting a growing body of evidence that, for women 30 years and older, detection of cervical intraepithelial neoplasia (CIN) 3+ lesions improves with HPV co-testing. The supporting studies also found that the risk of a high-grade lesion appearing 5 years following co-testing was equivalent to the risk seen with cytology samples alone taken at 3-year intervals. 8 The sensitivity of a single cytology test is only about 50%. 9 A patient’s risk of cervical cancer 18 months after 3 negative cytology tests is about 1.5/100,000. 10 The risk at 36 months following 3 negative cytology results is about 4.5/100,000. Annual screening would require almost 100,000 women to be screened to detect 3 additional cases of cervical cancer. 10
Additional benefits of the updated USPSTF guidelines. The updated strategy decreases the number of visits for patients and the number of colposcopies, minimizing harm and patient anxiety. The current management algorithms also recommend more conservative management of women in their early 20s who have reported abnormal cytology, as the likelihood of their lesion clearing within 12 to 24 months is high. 5 The recommendation does not call for high-risk HPV testing of women ages 21 to 29 because the infection is highly prevalent in this age group and is also likely to clear before any significant pathology arises. This avoids unnecessary and potentially harmful treatment of younger women. 11
What about the alternative screening guideline?
In early 2015, the American Society for Colposcopy and Cervical Pathology (ASCCP) and the Society of Gynecologic Oncology (SGO) co-sponsored an expert panel representing several specialty societies. The panel released interim guidelines for cervical cancer screening reflecting a growing body of evidence that favors HPV testing as the primary modality. 12 Additionally, in January 2016, these guidelines received an evidence-level B rating from the American Congress of Obstetricians and Gynecologists. 13 Primary HPV screening is also the topic of research and discussion for USPSTF’s pending 2018 update of cervical cancer screening strategies. 14
The alternative algorithm from the ASCCP and SGO recommends cervical cancer screening with HPV testing alone starting at the age of 25 and, if results are negative, repeating at 3-year intervals. 12 If a patient tests positive for any of the 14 identified high-risk HPV types, reflex cytology is indicated with a referral for colposcopy if an abnormality is identified. 12 If the cytology result is normal, follow-up with another HPV test in 12 months is recommended. 12
Over the last 12 years, multiple international studies have demonstrated the efficacy of high-risk HPV testing in primary screening for cervical cancer. 15 The most recent study conducted in the United States from 2008 to 2011—Addressing THE Need for Advanced HPV Diagnostics (ATHENA)—enrolled 42,000 women older than 25 years to compare the screening modalities of cytology alone, cytology and HPV testing combined, and HPV testing alone. 16 The purpose of the study was to determine the safety of the cobas HPV test as a co-test and as a primary screening modality in women older than 25 years. (Many HPV tests are commercially available, but only the cobas HPV test is FDA-approved for primary screening. 12)
ATHENA researchers concluded that HPV testing was more sensitive than cytology, but less specific. 16 The researchers also concluded that adding cytology to the HPV test increased the sensitivity by less than 5% and that HPV was better at detecting CIN 2+ lesions than cytology alone. 12,16 Another recently published study conducted at a tertiary care hospital with a smaller sample (1000 patients) corroborated the ATHENA results. 17
For patients in their late 20s, this alternative strategy may increase the number of subsequent colposcopies. However, during the clinical trials just described, the absolute number of colposcopies needed to detect high-grade disease was the same as seen with the current guidelines. This finding indicates that, with the current algorithm, clinically significant pathology due to high-risk HPV may be missed in the 25-to-29 age group. 8
Looking ahead. The alternative screening strategy is already being adopted in Australia, the Netherlands, and the United Kingdom. 15 For providers in the United States considering this alternative strategy, the recommendation is to initiate cervical cancer screening with cytology alone at age 21, manage results appropriately, and then transition the patient to primary HPV testing with the FDA-approved test at age 25. 12 This recommendation may be modified in the future. However the guidelines might change, patients will benefit only if the guidelines are implemented consistently in practice.
CORRESPONDENCE
Sabrina Hofmeister, DO, 1121 E. North Ave, Milwaukee, WI 53212; shofmeister@mcw.edu.