THE CASE
A previously healthy 35-year-old man with a one-week history of left-sided neck pain and fever as high as 104°F sought care at our emergency department. He was given a diagnosis of viral pharyngitis and discharged. He returned the next day and indicated that he was now experiencing drenching night sweats and weakness.
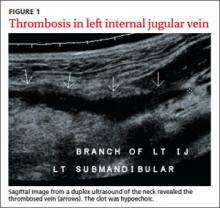
The patient was anxious, but not distressed. His temperature was 100.1°F; blood pressure, 113/65 mm Hg; heart rate, 150 beats per minute; respiratory rate, 18 breaths per minute; and oxygen saturation, 95% on room air. Head and neck examination revealed bilateral cervical lymphadenopathy with pronounced tenderness on the left side of his neck. Oral exam revealed dry mucous membranes, halitosis, and bilateral tonsillar enlargement without exudate. The cardiopulmonary exam was within normal limits. Lab tests showed a white blood cell (WBC) count of 5.9 x 109/L. An ultrasound of the neck revealed thrombosis in the left submandibular branch of the left internal jugular vein (IJV) (FIGURE 1).
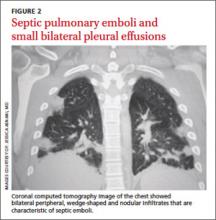
The next day, the patient remained febrile (102.8°F) and developed rigors, diarrhea, pleuritic chest pain, and an elevated WBC count (14.5). A blood culture grew gramnegative rods. The patient was started on piperacillin/tazobactam, and doxycycline was added to treat possible tick-borne infections. Computed tomography (CT) scans of the chest showed the presence of septic pulmonary emboli and small bilateral pleural effusions (FIGURE 2).
THE DIAGNOSIS
We made a diagnosis of Lemierre’s syndrome because our patient met all 4 criteria for the condition:1,2
• a recent oropharyngeal infection
• clinical or radiological evidence of IJV thrombosis
• isolation of anaerobic pathogens (mainly Fusobacterium necrophorum)
• evidence of at least one septic focus, most commonly in the lungs.
We changed the patient’s antibiotic therapy to intravenous (IV) meropenem. His WBC and fever improved, and on Day 10 he was discharged to complete a 28-day course of IV meropenem via a peripherally inserted central catheter.
DISCUSSION
Lemierre’s—A “forgotten” condition that’s making a comeback
In 1936, French microbiologist Andrew Lemierre formally characterized the syndrome in a review of 20 patients who had sepsis, metastatic pulmonary lesions, and isolation of Bacillus funduliformis (now known as F necrophorum).1,2 Other organisms that have been identified in this syndrome include Fusobacterium nucleatum, Candida, Staphylococcus, and Streptococcus.2
Before the antibiotic era, Lemierre’s syndrome was common and often fatal. But with the introduction of penicillin in the 1940s, the incidence of the syndrome dropped, and it eventually became known as “the forgotten disease.”2 Since the 1990s, however, there has been a marked resurgence of Lemierre’s syndrome.3 The incidence of Lemierre’s syndrome today is 0.6 to 2.3 cases per 1 million people per year, with a mortality rate of up to 18%.3,4
This resurgence of Lemierre’s syndrome has been linked to the restricted use of antibiotics for throat infections.3 (One study found the number of prescriptions written for antibiotics decreased by 23% from 1992 to 2000.5) Other factors cited for the increased incidence of Lemierre’s syndrome include improved identification of anaerobic organisms, more effective blood culture methods, and an increased awareness of this syndrome among clinical microbiologists.6
Diagnosis requires a high degree of suspicion
Lemierre’s syndrome typically occurs in healthy young adults. Pharyngitis is the most common initial symptom, occurring in 87% of patients.2 This is followed by a fever (102.2°F - 105.8°F) usually 4 to 5 days after the onset of sore throat.3 Other common symptoms include chills, dysphagia, dyspnea, chest pain, hemoptysis, cervical neck discomfort, arthralgia, malaise, and night sweats.2 Following suppurative thrombophlebitis of the IJV, infection spreads to other organ systems. Pulmonary involvement is the most common site (97% of cases).3 Other complications of this syndrome are listed in the TABLE.3
The differential includes mononucleosis
The differential diagnosis encompasses several common illnesses, including mononucleosis, Group A streptococcal pharyngitis, and peritonsillar abscess. However, while patients with these conditions might have a fever and an elevated WBC count, they typically would not have the pleuritic chest pain that is characteristic of Lemierre’s syndrome. In addition, while patients with peritonsillar abscess would have tonsillar exudates, patients with Lemierre’s syndrome would not likely have them.
Influenza is also part of the differential, although focal neck pain usually isn’t a finding in patients who have the flu.
Once other common illnesses have been ruled out, it’s important to have a high index of suspicion for Lemierre’s syndrome because the oropharyngeal infection may resolve by the time of presentation, and there may be few findings on physical exam.7 Therefore, suspect Lemierre’s if a patient comes in with neck pain and/or pleuritic chest pain and has a recent history of oropharyngeal infection and fever.