Applied Evidence
RADIOLOGY REPORT: An imaging guide to abdominal pain
When patients present with acute nontraumatic abdominal pain, knowing what disorders and which imaging modalities to consider is essential. Let...
Guy N. Gibson, DO
Dell P. Dunn, MD
Diagnostic Imaging, Ehrling Bergquist Clinic, Offutt Air Force Base, Neb (Dr. Gibson); Abdominal Imaging, David Grant Medical Center, Travis Air Force Base, Calif (Dr. Dunn)
guy.gibson.1@us.af.mil
The authors reported no potential conflict of interest relevant to this article. The views expressed here are those of the authors and do not reflect the official policy of the Department of the Air Force, the Department of Defense, or the US government.
Click here to view RADIOLOGY REPORT: An imaging guide to abdominal pain
Click here to view RADIOLOGY REPORT: Two radiologists offer 6 tips of the trade

CASE 1 ›
THE PATIENT: 28 year-old G0P0 woman
SIGNS & SYMPTOMS: Chronic pelvic fullness, acute lower abdominal/pelvic pain
A 28-year-old G0P0 woman with a history of chronic pelvic fullness presented with acute lower abdominal/pelvic pain. A pelvic exam showed mild cervical motion tenderness without vaginal discharge or palpable adnexal mass. Initial blood work was drawn and the patient was sent for a pelvic ultrasound with differential considerations including pelvic inflammatory disease, ovarian torsion, and intrauterine or ectopic pregnancy.
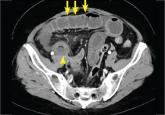
Transabdominal and transvaginal ultrasound (US) demonstrated unremarkable sonographic appearance of the uterus and bilateral ovaries. An evaluation of the adnexa was slightly limited secondary to multiple tortuous pelvic veins ( FIGURE 1 ). The adnexa were otherwise grossly unremarkable and there was a small amount of free fluid within the pelvis.
Lab values came back and were remarkable for mild leukocytosis. The patient had a negative human chorionic gonadotropin test.
Given the patient’s progressive symptoms and mild leukocytosis, the physician ordered a computed tomography (CT) scan of the abdomen and pelvis with contrast.
The CT of the abdomen and pelvis with contrast revealed multiple dilated (>4 mm) tortuous periuterine vessels, left greater than right ( FIGURE 2 , short arrows). There was concurrent dilation of the left gonadal vein, which measured up to 7 to 8 mm ( FIGURE 2 , long arrow). No other acute intra-abdominal or pelvic process was identified. A trace amount of simple appearing free fluid was noted.
WHAT'S YOUR DIAGNOSIS?
The patient was given a diagnosis of pelvic congestion syndrome. She was managed conservatively and referred to an OB/GYN, who recommended a venogram and left gonadal vein coil embolization. After the procedure, the patient improved.
DISCUSSION
Patients with pelvic congestion syndrome typically present with chronic (>6 months), non-cyclical pelvic discomfort or fullness. The pathophysiology is similar to varicoceles in men and can be caused by incompetent valves, compression of the left renal vein by the superior mesenteric artery, or venous obstruction from an anatomic variant such as a retroaortic left renal vein. Treatment options include gonadal vein embolization and laparoscopic ligation.
Key imaging characteristics: Ultrasound, magnetic resonance imaging, and CT may show tortuous, dilated pelvic veins that measure >4 mm or a gonadal vein that measures >7 mm, consistent with pelvic or ovarian varices.
If there is clinical suspicion or imaging features suggestive of pelvic congestion, patients may require a pelvic venogram. Because established imaging criteria vary and initial imaging assessments can appear normal, pelvic congestion syndrome ultimately remains a clinical diagnosis.
CASE 2 ›
THE PATIENT: 64-year-old man with a history of diverticulosis
SIGNS & SYMPTOMS: Left lower quadrant pain
A 64-year-old man with a history of diverticulosis presented with 3 days of worsening left lower quadrant pain. Given the patient’s progressive symptoms and pain out of proportion to exam, acute diverticulitis was suspected. A computed tomography (CT) scan of the abdomen and pelvis with contrast was ordered to exclude complicating factors.
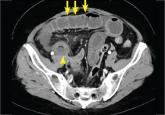
Axial CT images through the left lower quadrant demonstrated a 2.5 cm fat-containing ovoid lesion ( FIGURE, star) with hyperemic rim ( FIGURE, short arrows) abutting the lateral wall of the sigmoid colon with mild surrounding inflammatory change ( FIGURE, long arrow).
There was no evidence of superimposed bowel obstruction, free air, or abscess formation. Scattered colonic diverticula were noted, without adjacent inflammatory change to suggest acute diverticulitis.
WHAT'S YOUR DIAGNOSIS?
The CT findings were consistent with a diagnosis of epiploic appendagitis. Subsequent lab work demonstrated no evidence of leukocytosis and a normal lactate value.
Given the benign and self-limiting nature of epiploic appendagitis, the patient was managed conservatively with oral anti-inflammatory medications (600 mg ibuprofen PO every 8 hours for 4-6 days) and released from the clinic with return precautions. Follow-up in 7 days demonstrated near-complete resolution of the patient’s symptoms.
DISCUSSION
Epiploic appendagitis is typically a nonsurgical, self-limiting process resulting from torsion of one or more epiploic appendages along the sigmoid, descending, or right hemicolon with resultant vascular occlusion that leads to ischemia.
Epiploic appendage ligation and resection is rare and usually reserved for when conservative management fails or there is new or worsening symptoms such as fever, progressive pain, or refractory nausea and vomiting.
Key imaging characteristics: 2-3 cm ovoid, fat-containing paracolic mass with thickened peritoneal lining and periappendiceal fat stranding. Classic features include a hyperattenuated central dot within the appendage corresponding to the thrombosed draining vein.
When patients present with acute nontraumatic abdominal pain, knowing what disorders and which imaging modalities to consider is essential. Let...
