THE CASE
A 57-year-old Hispanic man sought treatment because he had been feeling tired for a few weeks. He had not seen a physician for 15 years. When he came in, his temperature was 98.8°F, blood pressure was 132/82 mm Hg, pulse was 82 beats/min, respiration rate was 16 breaths/min, and oxygen saturation was 93% on room air. Examination of the head, neck, and respiratory and cardiovascular systems was normal. Skin examination showed petechiae and bruising on his abdomen, left ankle, right thigh, and bilateral shin area. His abdomen was nontender with no organomegaly. There was no focal neurological finding or spinal tenderness. Our patient had no chills, chest pains, shortness of breath, headache, dizziness, or loss of consciousness. There was no hematemesis, melena, hematuria, edema, or weight loss. He had no medical or surgical history and denied substance abuse or taking any medications recently; he did use alcohol previously.
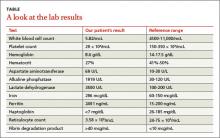
Results of some initial lab tests were abnormal, including a decreased white blood cell count (5.82/mcL), platelet count (29 x 103/mcL), hemoglobin (8.6 g/dL), and hematocrit (27%) (TABLE). A peripheral blood smear showed decreased normocytic red blood cells and scattered schistocytes. His prostate-specific antigen (PSA) level was elevated at 212 ng/mL.
The patient’s coagulation profile was normal, and his von Willebrand factor (vWF) protease (ADAMTS-13) level was within normal limits (13.83). Antineutrophil cytoplasmic antibody and antinuclear antibody tests were negative. Testing for pulmonary embolism was negative, as was testing for human immunodeficiency virus. An abdominal ultrasound was normal, as well.
THE DIAGNOSIS
Based on our patient’s abnormal blood test results and the presence of petechiae and bruising, we diagnosed thrombotic thrombocytopenic purpura (TTP). The patient’s elevated PSA prompted us to order computed tomography of the chest and abdomen, which showed an enlarged prostate gland and mixed lytic sclerotic lesions in T3 to T5 and T9 vertebrae and in his ribs. A bone marrow biopsy revealed metastatic prostatic adenocarcinoma and a bone scan confirmed multiple metastases in the spine, pelvis, and shoulders.
DISCUSSION
TTP is a rare disorder of increased clotting in small blood vessels throughout the body that can include thrombocytopenia, microangiopathic hemolytic anemia (MAHA), fever, renal dysfunction, and neurological deficits.1 It’s important to maintain a high index of suspicion for TTP because the condition is a hematologic medical emergency that can quickly cause multiorgan failure and death.2
Almost always an acquired condition, TTP can be idiopathic or secondary to another condition, such as collagen vascular diseases, transplants, certain drugs, infections, pregnancy, or cancer.3 In idiopathic TTP, the cause of the condition is believed to be reduced activity of ADAMTS-13, the protease that breaks vWF into smaller pieces—thus preventing the formation of unnecessary blood clots.
In cancer-associated TTP, which could be a complication resulting from chemotherapy or a manifestation of cancer itself,3 ADAMTS-13 level is normal and the condition is likely the result of an increased tumor cell load, which leads to endothelial damage and fragmentation of red blood cells (RBC) as they traverse the injured microvasculature.4 In an analysis of 154 cases of “solid” cancer-related MAHA, Lechner and Obermeier5 found 23 cases were related to prostate cancer, as was the case with our patient.
Treatment for TTP is plasma exchange. The mortality rate of untreated TTP can exceed 90%, but plasma exchange therapy has reduced that rate to <20%.6 It has been suggested that proteolysis of vWF may play a central role in the efficacy of plasma exchange for TTP.7
Our patient was hospitalized and received 2 units of packed RBCs. He also received plasma exchange for 9 days with minimal response. On Day 5, our patient was started on leuprorelin and parenteral steroids. Soon after, his platelet count rose to 33 × 103/mcL and lactate dehydrogenase decreased. He was discharged approximately one week after the steroids were started.
After several months of outpatient treatment with leuprorelin and bicalutamide, the patient’s platelet count normalized to 212 × 103/mcL (from 29 × 103/mcL), alkaline phosphatase decreased to 402 U/L (from 1919 U/L), and PSA levels trended downward to 8.63 ng/mL (from 212 ng/mL). He continued to receive care from our oncology clinic for the next several months and his PSA level continued to decline. However, at his last few visits, his PSA level had trended up, suggesting progression of his prostate cancer. The patient has not followed up with our clinic recently.
THE TAKEAWAY
Suspect TTP in patients who present with unexplained petechiae and bruising, and whose blood work reveals thrombocytopenia and MAHA.2 Patients with TTP who do not respond to plasma exchange should be evaluated for underlying cancer or other potential secondary causes.3 Patients with cancer-associated TTP may respond to steroid therapy.