- Tell patients with type 2 diabetes mellitus (T2DM) that chromium and fiber appear to have a beneficial effect on glycemic control, while the benefits of other dietary supplements are not known. C
- Recommend acupuncture for patients with T2DM and peripheral neuropathy, bladder dysfunction, or symptoms of other comorbidities that have not fully responded to conventional therapy. B
- Advise patients that biofeedback and meditation are more likely than other types of stress reduction to improve glycemic control. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Integrative medicine—an approach that combines conventional and alternative therapies with an emphasis on natural, less invasive evidence-based options—is well suited to the management of complex chronic diseases like type 2 diabetes mellitus (T2DM). And we’ve found that patients with T2DM are increasingly interested in integrative strategies, most of which involve self-management and lifestyle changes. They’re often motivated by the desire to limit the number of medications they’re taking or to avoid diabetes drugs entirely. In many cases, patients also hope to alleviate symptoms of comorbidities that have not fully responded to conventional treatment, such as peripheral neuropathy, bladder dysfunction, and gastroparesis.
As a family physician, you’re likely to be asked about unconventional approaches to diabetes and to be in a position to recommend alternative therapies in conjunction with pharmaceutical management of T2DM. In both cases, you need to know which integrative strategies have evidence to support their use. We created the text and tables that follow with this in mind.
Nutrition and weight loss: What works?
To reduce cardiovascular disease risk factors, patients with T2DM are advised to eliminate trans fats and to limit saturated fat to <7% of total caloric intake. A moderate weight loss (5% of body weight) has been found to improve insulin action, decrease fasting blood glucose (FBG) concentrations, and reduce the need for diabetes medications.1,2 One small retrospective cohort study (N=72) found that a 10% weight loss was associated with a reduction in glycosylated hemoglobin (HbA1c) of 0.81 percentage points.3 Weight maintenance is also an important element of diabetes management, even for patients who have not been able to lose their excess weight.2
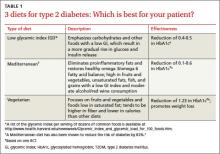
American Diabetes Association (ADA) guidelines do not endorse a specific diet. But patients often ask for dietary advice and want to know how specific diet plans and food choices will affect glycemic control and comorbid conditions. You can present the evidence (TABLE 1)4-6 of the effectiveness of a low glycemic index (GI) diet, a Mediterranean diet, and a vegetarian diet and point out that the best diet for a particular patient is the one best suited to his or her lifestyle and dietary goals.
Low glycemic index diet. The 2013 ADA guidelines acknowledge that a dietary regimen with a low glycemic index (GI) may be more beneficial for glycemic control than a diet based on total carbohydrate count alone.7
A Cochrane review of 11 small studies found a reduction in HbA1c of 0.5 (95% confidence interval [CI], -0.9 to -0.1; P=.02) in patients with T2DM who followed a low GI diet for 4 weeks or more. Patients on this diet also had a significant reduction in hypoglycemic events compared with those on other dietary regimens;4 one of the studies included in the meta-analysis also found a statistically significant increase in high-density lipoprotein cholesterol (HDL-C) in those on the low
GI diet.8
Mediterranean diet. Rich in fruits and vegetables and unsaturated fats, fish, and grains with a low GI, the Mediterranean diet has a higher carbohydrate and fat content than a portion-controlled diet formerly recommended by the ADA. (As noted earlier, current ADA guidelines do not recommend a particular diet).
A systematic review of 5 randomized controlled trials (RCTs) (N=1077) found improved glycemic control in patients on a Mediterranean diet compared with those on other commonly used diets, such as low fat and portion-controlled regimens. Fasting blood glucose (FBG) fell between 7 and 40 mg/dL and HbA1c by 0.1 to 0.6 in studies that ranged from 6 months to 2 years.5 The effectiveness of the Mediterranean diet, despite its higher carbohydrate content, suggests that treating systemic inflammation may help to reduce insulin resistance and hyperglycemia. The effectiveness of the Mediterranean diet--despite its higher carbohydrate content--suggests that treating systemic inflammation may help to reduce insulin resistance and hyperglycemia.
Vegetarian diet. Vegetarian and vegan diets also offer potential benefits in the management of T2DM—including the fact that they tend to be lower in calories than other dietary regimens and therefore more likely to promote weight loss. In one 22-week RCT (N=99), those who were randomized to a low-fat vegan diet lost more weight (6.5 vs 3.1 kg; P<.001) and had a larger decrease in HbA1c (-1.23 vs -0.38; P<.01) and low density lipoprotein cholesterol (LDL-C) (-22.6 vs -10.7 mg/dL; P=.02) compared with those following a portion-controlled ADA diet. Glycemic change correlated with the change in body weight.6